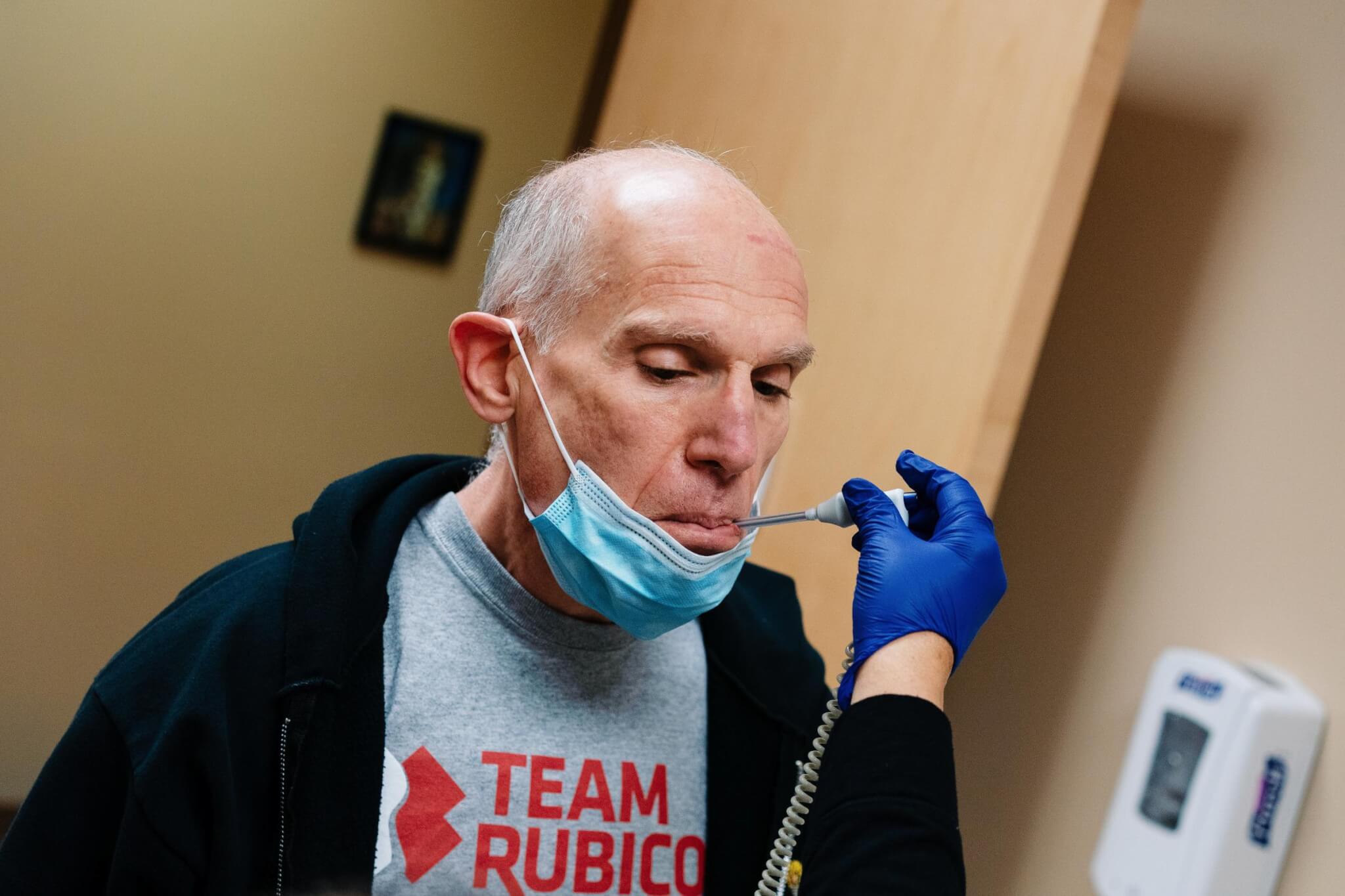
When Team Rubicon volunteers first arrived at the Navajo Nation in Kayenta, Arizona, this spring they had no idea it would be the organization’s largest medical operation to date. Or, that it would be the beginning of what is likely to become a whole new service sector for Team Rubicon: providing medical support and relief within the United States, not just internationally. Those volunteers—or Greyshirts—also had no idea how many lives they’d touch.
That was in early April. By the time the group demobilized in mid-July, much had changed.
At about 27,000 square miles, and spanning parts of New Mexico, Arizona, and Utah, the Navajo Nation is the largest Native American reservation in the U.S. With more than 300,000 enrolled tribal members, including nearly 157,000 who live on the reservation, the tribe is the second largest in the country behind the Cherokee tribe. It is also home to a proud contingent of veterans: In addition to the famed Navajo codebreakers of World War II, the tribe boasts approximately 12,000 veterans among its ranks. The Navajo Nation may be huge; its people may be many and patriotic, but those things didn’t spare it from the coronavirus pandemic. In May, it had the highest per-capita COVID-19 rate in the U.S. The people of the Navajo Nation were experiencing unimaginable losses.
The staggering number of people impacted by the coronavirus is why Team Rubicon deployed 128 Greyshirts—including 47 medical volunteers—to the Nation early this spring. Over the course of more than 90 days, the Greyshirts spent more than 15,000 hours volunteering and served more than 3,000 patients.
We sat down to found out why five medical Greyshirt volunteered, and how their work on the Navajo Nation changed them. Early on in the COVID-19 outbreak, U.S. Navy veteran and nurse Charlotte Semple went to New York City—then the epicenter of the pandemic—on a paid nursing assignment. She returned home thinking she’d rather volunteer. So, when the opportunity to deploy to the Navajo Nation with Team Rubicon arrived, the nurse jumped at the chance. In mid-June, she headed to Arizona where she worked in the respiratory care unit of Chinle Hospital’s COVID unit for two weeks. The work had such an impact that she returned for a second stint. What was the hardest thing about serving at the Navajo Nation?
Maybe lockdown. I’m a big outdoors girl so it was kind of hard to be there, in this amazing place, and not able to go to explore it.
As far as the experience? The staff at the hospital were super welcoming and super helpful and friendly, and glad you’re there, so that was good.
What was the most impactful thing that happened during your deployment?
I think the numbers that have been affected there, and the number of people who know someone who died or has been extremely ill, had a big impact. And, it’s a very small hospital. Anybody serious has to be flown out, so their ER is incredibly busy.
Is there one thing you experienced that will stick with you forever?
At the Chinle Hospital they do what they call a “calling Dr. White” when we discharge somebody. The staff would line up and clap for the person as they went by in a wheelchair and exited the building. Even the maintenance staff and security, when they heard the announcement, would go to the other side of the parking lot and see the person off. That was very touching. Andrew Motz is a mechanical engineering major at Massachusetts Institute of Technology, where he’s also in Navy ROTC and works as an EMT with the MIT ambulance service. This summer he decided to put that training to good use with Team Rubicon.
Motz deployed to the Navajo Nation operation not once but twice—for 10 days each time—where he served as an EMT at the Alternate Care Site in Chinle, the ERs at Chinle and Kayenta, and with the EMS offices in Kayenta and at Inscription House Health Center.
What was the most important thing you learned during your time at the Navajo Nation?
This opportunity was very eye-opening in regards to what rural medicine looks like. I live in Seattle, where we have Harborview and Swedish Medical centers; on top of that we have Seattle Children’s Hospital. I also work and go to school in Boston where there are five Level 1 trauma centers in our service area. So, it was really eye-opening to see how rural clinic medicine worked, and to see how things change when your closest medical facility is an hour away. It has really been revealing to see how much harder it is to get good medical care when living in such rural areas.
How did your service at the Navajo Nation change you?
What this op made me realize was how much of an effect we can have on people just by being there. Even when we had slow shifts, the locals, especially on the EMS side, were grateful for us being there. Our presence allowed them to take days off and rest, something that they hadn’t had in months. And it showed them that they’re not alone. Specifically in the EMS system; especially at Inscription House. They had a lot of individuals come down sick, or quit because they didn’t want to have to worry about exposure. They were really short staffed.
I think what we did there actually made a difference, but to me the best takeaway was from my time at Inscription House: the positive effect we had on their morale; that we were there to help and that they weren’t in it alone.
A paramedic in Fairbanks, AK who also teaches in the paramedic program at University of Alaska Fairbanks, Alford spent a month deployed to the Navajo Nation working as a paramedic in the ER.
Why did you decide to deploy with Team Rubicon to the Navajo Nation?
While I was still on our medical operation in Santa Clara I had friends volunteering in Arizona who were telling me about the situation on the ground. The Navajo Nation was affected so deeply, and I could relate to many of the challenges they were facing since there are similarities to working in Alaskan communities. Working and living in a smaller community makes it more likely you’ll have ties to your patients through friends or family, and this only increases the emotional toll. The fact that they were also short staffed, due to COVID, and had multiple staff out sick with the virus—some in critical condition—was putting an even heavier burden on healthcare providers.
Knowing that I had the necessary background and skills to help, and the time to give, how could I not offer to serve? What was the hardest thing about serving in Kayenta?
Leaving this operation was the hardest part for me. After a month of working closely with both full-time staff and contractors, strong bonds were formed. I became a part of their team as we all worked together to provide the best care possible in new and challenging circumstances. I connected with many patients, some of whom I treated on multiple occasions. Becoming integrated into that community, working with some amazing people, and the fact that they would be continuing long after I left made this one of the more challenging ops to leave.
What was the most impactful thing that happened during your deployment?
There wasn’t any one event or person that impacted me the most, but rather the community as a whole. And, countless moments: Local nurses and health techs sharing their food, culture, and stories. ER staff taking time to explain cultural nuances or how to better serve and treat elders in the community and teaching me Navajo phrases so I could show patients I cared in their own language. Challenging moments, like offering an ear to a doctor who was feeling overwhelmed at the enormity of the situation, with no end in sight. Then taking a deep breath together, checking our PPE, and walking back in to treat yet another critical patient with COVID-19. Nurses who wanted to make sure I took time reset and got to see the natural beauty in the area. They took me out to hike and climb on the mesas and to breathe in the wind and fresh air so we could all go back the next day and keep serving. Retired U.S. Air Force physician Stanley Chartoff, MD, deployed with Team Rubicon to the Navajo Nation in April. Over the course of three weeks Chartoff served alongside IHS doctors in the ER caring for patients with general illnesses and traumas and also with the coronavirus. Dr. Chartoff appreciated being able to employ the COVID-19 expertise he’d recently gained working as an emergency room physician at University of Connecticut’s Hartford Hospital. What was more fascinating for Chartoff, however, was how his experience as a doctor in the Air Force served him at the Navajo Nation.
What was your role at the Navajo Nation?
I’m an emergency physician, so I provided direct medical care as an ER doctor. I assisted the other doctors—the paid doctors who were there with IHS—in taking care of patients. A lot of the regular physicians are more family practice doctors, so they weren’t quite as familiar with COVID-19, and especially with really sick patients. I assisted them with the care of those patients, and because of my recent experience in Connecticut, was also able to help them learn more about treating COVID-19. Did your experience in the military help in your service at the Navajo Nation?
Actually quite a bit. In the military my role was that of vital care transport doctor. I took care of patients on airplanes as we were transporting them out of Afghanistan and Iraq, so I had a lot of critical care background, which I don’t get much of now in my primary job. That was particularly true of taking care of ventilators. When I got to Navajo Nation, I discovered they don’t have any respiratory therapists on staff in their hospital. So, I had to set up and run my own ventilators while I was there. That military training I had really, really helped me.
What was the hardest thing about serving on this operation?
I suppose the emotional aspect of it. The Navajo are such wonderful people, and having to send a lot of them home, especially the ones who weren’t sick enough to be transported to a hospital, and also knowing that they were going back to not ideal conditions—many told me they live in communal housing with elderly people or in homes without running water—was very hard.
I also cared for a lot of families. I had to intubate a gentleman one day, then two days later I intubated his mother. That’s not something I am used to seeing. A registered nurse from Phoenix, and the lead faculty for an RN to BSN program at Grand Canyon University, Alicia Shields first deployed to the Navajo Nation on May 1. She was still there when Team Rubicon demobilized on July 10. During her more than two month stint, Shields supplemented staffing in the ER on the night shift, then spent the last three weeks of her deployment as a charge nurse. (Read her recent reflection The 91-Day Greyshirt.) Why did you decide to deploy with Team Rubicon to the Navajo Nation?
The Navajo Nation has a very special place in my heart. I spent seven years living and working on the Navajo Nation; my daughter even went to first grade at Tsehootsooi Primary School in Fort Defiance. I have some close friends who are from the Navajo reservation and it was heartbreaking to see how COVID-19 has devastated families and communities. I wanted to give back to the place that had given me so much and so many memories.
What was the most important thing you learned during your time serving at the Navajo Nation?
Being familiar with the culture I pretty much knew what to expect. What being here did do was to reinforce to me the concept of K’e. K’e is a Navajo concept that is based on respect, responsibility, and relationships. Seeing the staff here care for one another and for the community showed that K’e is a part of them. They also showed it when they accepted me as part of their team. On night shift we had such good teamwork that you would have thought we worked together for years.
How did your service at the Navajo Nation change you?
Serving here also made me realize how much I have missed the front line. I left the bedside for leadership and then academia, and being here, on the frontline doing bedside care, reminded me just how much I have missed it.
What was the most impactful thing that happened during your deployment?
There were so many impactful moments. On my first shift I was logging into the computer and heard a familiar voice. It was PJ! We had worked together almost 10 years ago when I did a contract in Gallup at the IHS hospital there. It was so amazing to see a familiar face.
Time after time patients would see the Team Rubicon logo on my scrubs and thank me for coming here to help out. People were very appreciative and they let us know it.
I met many new friends both inside and outside of Team Rubicon who have had a profound impact on me, and we will forever be friends. I am really looking forward to serving with them again on future ops. Some of the people we worked with have also become Greyshirts and I cannot wait to see them on an op. Big, Bold, and Hit Hard
Big, Bold, and Hit Hard

Charlotte Semple, RN


Andrew Motz, EMT

Rachel Alford, EMT-P


Stanley Chartoff, MD

Alicia Shields, RN


Meet the medics in grey who served the Navajo Nation
Written by Julie H. Case